AI vs. Human Claims Intake: What You Need to Know

Amir Prodensky
CEO
Dec 18, 2025
13 min read
How AI and human agents perform in real insurance claims
Claims intake is the first step when a policyholder reports a loss. It’s crucial because it sets the tone for the entire claims process and impacts customer satisfaction. Today, more insurers are turning to AI voice agents and automation to speed up and simplify this step.
You’ll see how AI-driven claims intake stacks up against human agents by looking at benchmarks from 15 insurance companies. This practical guide focuses on tools, performance, integration, and future trends – everything you need to know to make informed decisions.
By the end, you’ll learn how to improve your claim intake process with AI, balancing efficiency and customer care.
What are AI voice agents and how do they work in insurance claims intake?
AI voice agents are smart digital assistants that chat with you in real time. They use natural language processing (NLP) to understand your words, automatic speech recognition (ASR) to hear you clearly, machine learning (ML) to get better over time, and text-to-speech (TTS) to respond naturally.
Unlike old-school interactive voice response (IVR), AI voice agents grasp natural language, remember context across turns, handle multiple languages, detect emotions, and adapt on the fly.
In insurance claims intake, these agents handle tasks like:
First Notice of Loss (FNOL) reporting.
Lead qualification.
Appointment booking.
Claim status updates.
Billing questions.
Fraud flagging.
Preliminary eligibility checks.
You’ll find platforms like Lindy (no-code rapid builds), VAPI (developer-friendly APIs), , Synthflow, Cognigy, EMA, Talkie.ai, Yellow.ai, Kore.ai, and Voiceflow powering these agents.
These tools offer 24/7 service, call summaries, automated claim docs, ID verification, CRM and claims system integrations, plus compliance with standards like HIPAA and GDPR. One standout is Strada, built just for insurance. Its AI models get insurance jargon and workflows, giving you accurate, smooth FNOL calls, renewals, and service requests over phone and SMS.
Strada plugs right into AMS, CRM, and claims systems, turning conversations into automated actions with its Strada Workflows platform, making it more than just another voice AI.
With Strada, you get a trusted partner for claim intake outsourcing and the best voice AI for claim intake automation.
Yet, before we compare AI to humans, let’s get clear on what AI voice agents actually are and how they fit into insurance claims intake. Once this clicks, everything else makes more sense.
How does human claims intake work, and what are its challenges?
You’re probably familiar with the traditional claim intake process. Usually, claims adjusters or call center agents answer live calls from customers.
They gather all the necessary information and manually enter it into claims management systems. Then, they use their judgment to decide how to triage and route each claim.
If a case is complex, they escalate it to specialized teams. This hands-on approach relies a lot on human skill and experience.
Several key metrics help track how well this process works. These include:
Average Handle Time (AHT) → How long each call or claim takes.
Cost Per Claim Intake → The expenses involved in processing each claim.
Error Rate → Mistakes like missing data or input errors.
First Contact Resolution Rate → How often claims are handled without needing a callback.
Customer Satisfaction (NPS) → How happy customers are with the experience.
Despite the personal touch, there are challenges. Keeping a large team staffed is expensive, and employee turnover keeps rising. During disasters or peak claim times, operations get strained because you need more agents quickly.
Agents sometimes don’t stick closely to schedules or scripts, leading to uneven service. Data entry errors can slip through, and extensive training is required both at the start and ongoing. Scaling to meet sudden volume spikes is tough, too.
That’s where technology steps in, especially AI voice agents. Unlike human teams, AI agents can scale effortlessly, work 24/7, and handle many calls at once without getting tired or distracted. They deliver consistent results without shift changes or breaks.
For example, Strada’s AI voice agents help ease pressure during busy periods by managing claim intake calls autonomously. This lets human agents concentrate on more complex or sensitive cases, improving overall efficiency and customer experience.
Now that you know how AI voice agents work, it helps to step back and look at the traditional approach. Understanding how human-led intake operates sets a clear baseline for comparison.
How AI and human claims intake compare: speed, accuracy, cost, and customer experience
Here, you’ll learn how AI stacks up against human agents when handling claims intake, focusing on speed, accuracy, cost, and customer experience.
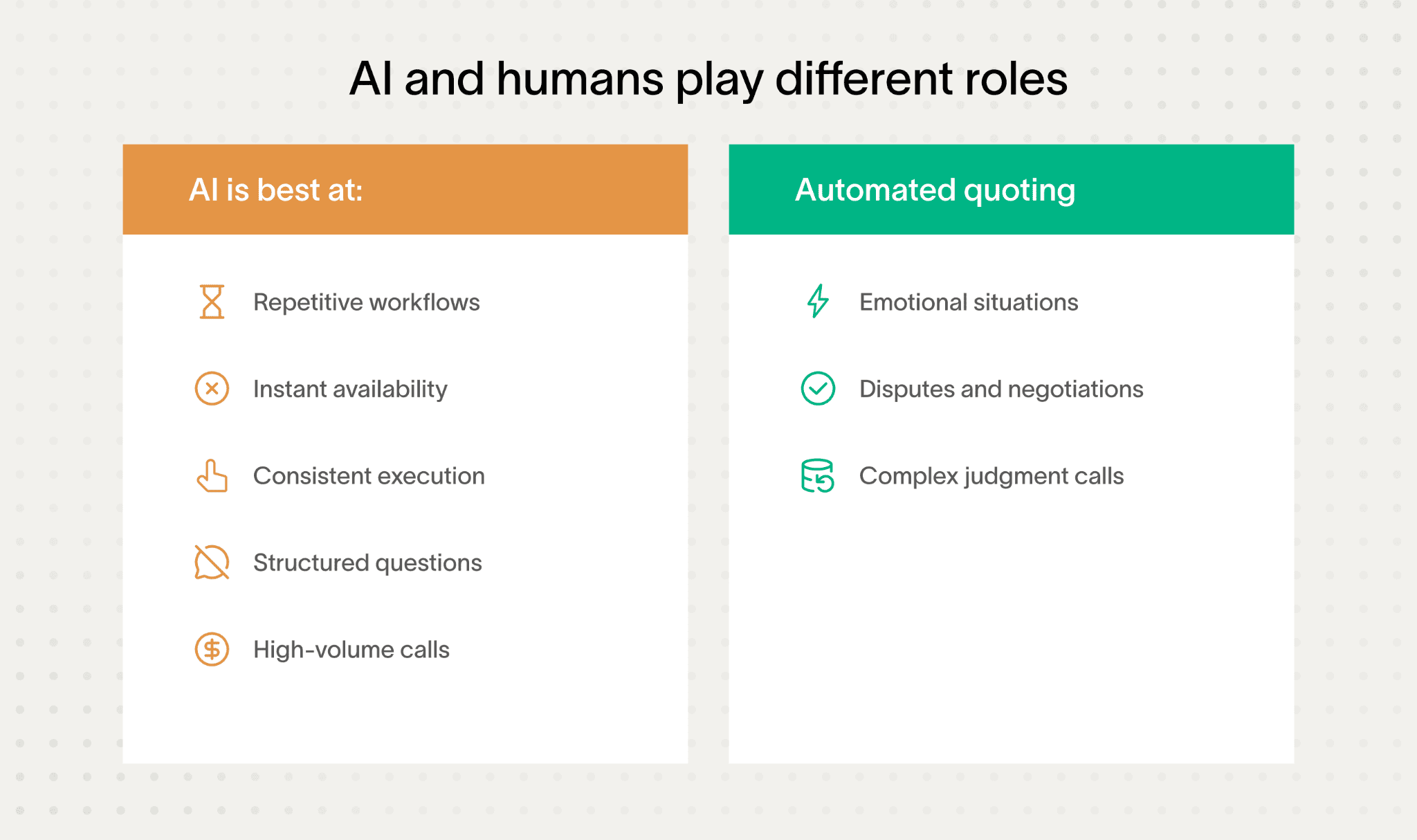
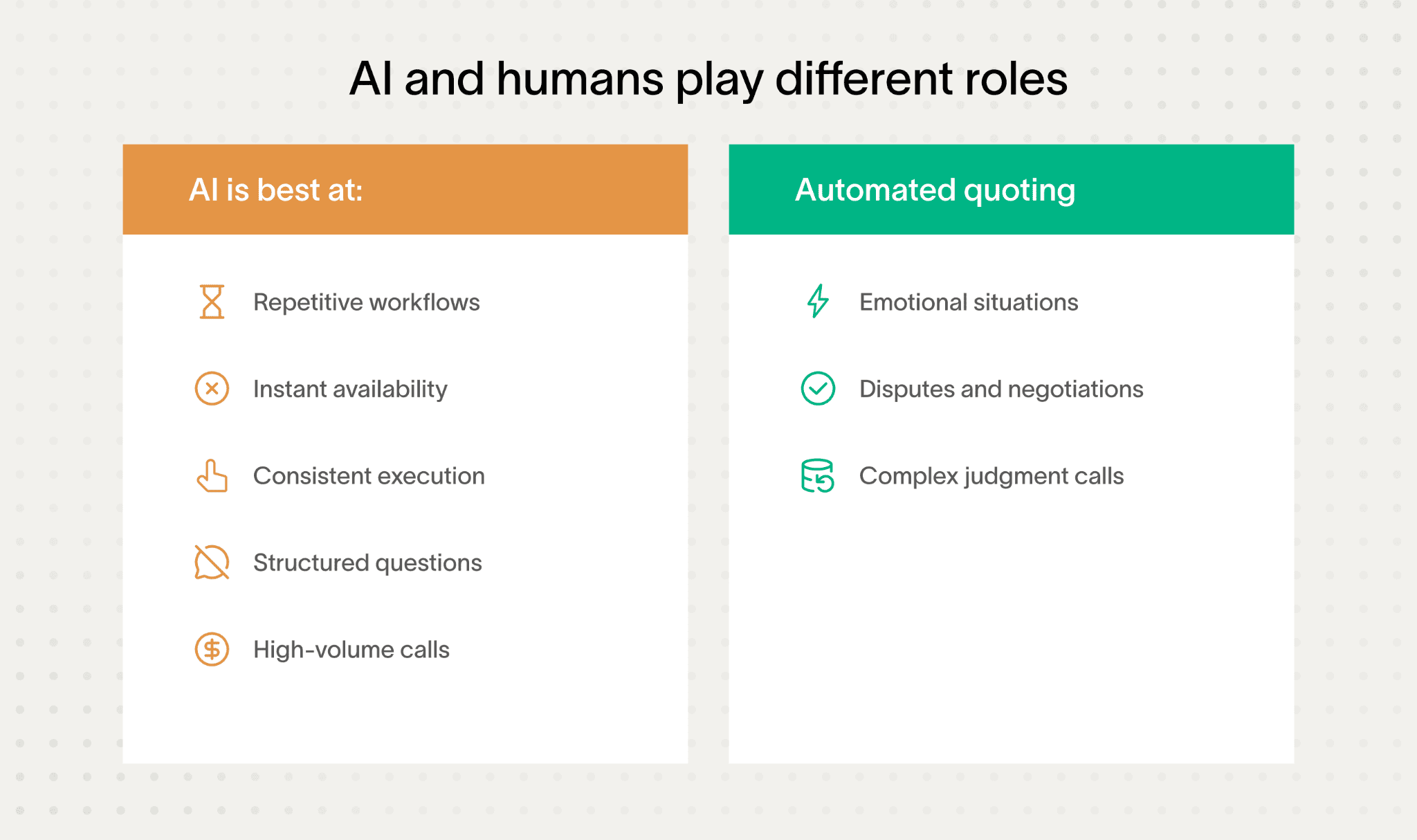
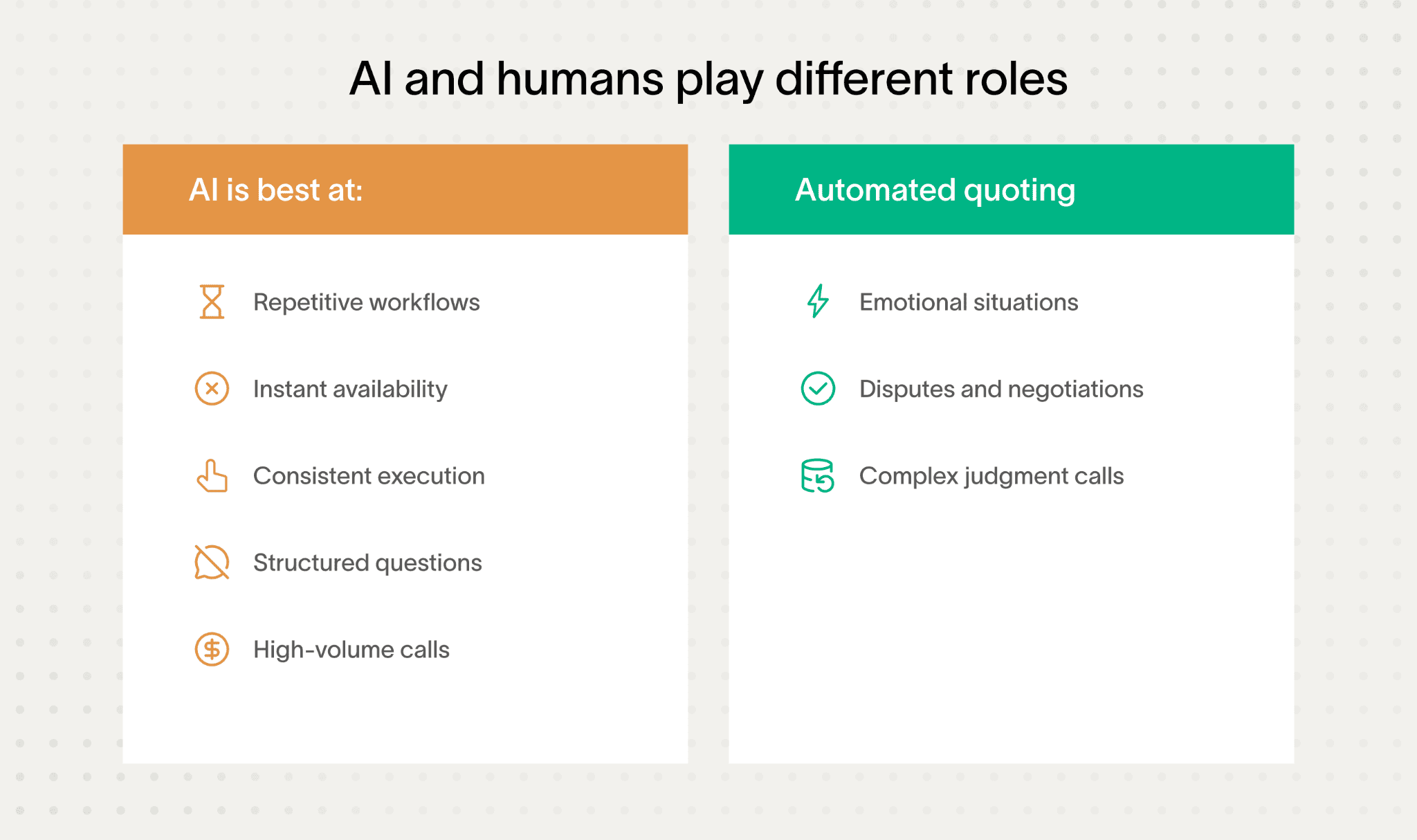
This isn’t a winner-takes-all story.
Each side shines in different moments.
Let’s break it down.
Speed
Speed is one of the clearest differences between AI and human claims intake. Automation removes manual steps and eliminates queues during high call volumes:
Shorter intake time → Structured data capture cuts average claim intake from around 18 minutes to under 6 minutes in real-world cases.
Parallel call handling → AI can manage multiple calls at once, preventing delays during peak demand.
No human constraints → AI doesn’t require breaks, shift changes, or recovery from fatigue.
This makes AI especially effective during traffic spikes, when human teams struggle to scale fast enough.
Accuracy
AI uses domain-specialized speech recognition (ASR) and natural language understanding (NLU) models trained on insurance-specific terms.
This delivers over 90% accuracy in transcription and intent recognition, which means fewer errors, less rework, and fewer callbacks. Humans excel when it comes to complex judgments and sensing emotional cues.
However, their consistency can vary more compared to AI’s steady performance.
Cost efficiency
Cost efficiency highlights a key structural difference between AI and human claims intake. AI pricing scales with usage, while human teams come with fixed labor costs:
Usage-based pricing → AI typically runs on pay-per-minute models (around $0.07 per minute) or low-cost subscriptions starting near $29 per month.
Lower overhead → AI removes salaries, benefits, onboarding, and ongoing training expenses.
No surge penalties → AI doesn’t require overtime pay or temporary staffing during peak volumes.
This keeps costs predictable and scalable when claim volume increases.
Customer experience
AI provides fast, consistent responses in multiple languages, Spanish, French, Mandarin, Hindi, with predictable service-level agreements. But humans still shine in handling emotionally sensitive cases and complex disputes, building rapport in ways AI can’t match yet.
Here’s a quick look at benchmarks from 15 insurance companies:
Average Handle Time (AHT) → AI averages around 5-6 minutes; humans around 15-18 minutes.
Error Rates → AI below 10%; human error rates vary more widely.
Customer Satisfaction (NPS) → Comparable scores, with humans leading slightly in empathy-driven cases.
Scalability → AI handles spikes without extra cost; humans need more staffing.
Throughput Per Channel → AI supports phone and SMS seamlessly; humans limited to capacity.
Cost Per Claim Intake → AI at least 1x more cost-efficient, often more.
Strada’s voice AI stands out with over 85% of calls answered, near-zero hold times, and improved call containment rates. It’s also multilingual and omni-channel, enabling claims intake via phone and SMS without delays. This gives customers timely, smooth experiences while keeping costs low.
To make this easier to apply in real operations, it helps to step back and look at a clear, side-by-side summary of how AI and human intake actually differ in practice.
Area | AI voice agents | Human agents | Practical takeaway |
Speed | Consistently fast | Slows down under load | Faster FNOL improves first impressions |
Availability | 24/7 coverage | Limited to shifts | No missed claims after hours |
Cost model | Usage-based | Fixed labor costs | Easier cost control at scale |
Accuracy | High for structured data | Varies by agent | Less rework later |
Peak volumes | Scales instantly | Needs overtime or hiring | Critical during catastrophes |
Emotional cases | Escalates when needed | Strong empathy | Hybrid approach works best |
Both approaches have strengths and trade-offs. Let’s put them side by side and see how AI and human agents stack up where it really counts.
What criteria should insurers use to evaluate AI voice agents?
When choosing the best voice AI for claim intake automation, you want a solution that works flawlessly and fits your unique needs. Here’s what you should focus on to make a smart decision.
Infrastructure reliability
Reliability is non-negotiable in claims intake. If the system drops calls or responds slowly, customer trust disappears instantly.
That’s why insurers focus on a few core infrastructure requirements:
High availability → Look for guaranteed uptime of 99.9% or higher to avoid dropped or failed calls.
Low latency → Response times should stay under 300–500 milliseconds to keep conversations natural and uninterrupted.
Built-in redundancy → Automatic failover ensures another server takes over if one goes down.
Deployment flexibility → Cloud setups offer speed and scalability, while on-prem options give insurers tighter control.
Strong infrastructure keeps claims intake stable during peak demand and unexpected outages, protecting both service quality and operational continuity.
Security & compliance
Insurance data is sensitive.
Make sure the AI platform meets high standards like SOC 2 Type II and ISO 27001. If you handle health or personal data, HIPAA compliance is essential. For European customers, GDPR must be covered, and if payments are involved, PCI-DSS should be in place.
The best platforms use AES-256 encryption for data at rest and in motion. They also support real-time redaction of sensitive info like PII or PHI, plus workflows that capture customer consent and create unchangeable audit trails to satisfy regulators.
Integration capabilities
Strong integrations determine whether AI actually fits into your operations or becomes another silo. Claims intake only works at scale when systems share data smoothly.
That’s why insurers focus on a few integration essentials:
Core system connectors → Native integrations with CRMs like Salesforce and Microsoft Dynamics 365.
Policy and claims platforms → Support for systems such as Guidewire, Duck Creek, ClaimCenter, and Xactimate.
Telephony compatibility → Easy connection to platforms like Twilio or Genesys for call handling.
Workflow automation hooks → APIs and webhook callbacks to trigger updates and actions across systems in real time.
When integrations are solid, claims data flows automatically, reducing manual updates, errors, and delays across the entire intake process.
Insurance-specific workflows support
Choose AI that’s smart about insurance tasks. It should handle First Notice of Loss with guided questions, prioritize claims, send renewal reminders, answer billing queries, schedule payments, collect documents, flag fraud, and even make proactive outbound calls.
Having these pre-built saves you time and ensures smoother customer experiences.
To make this practical, here’s a quick checklist of must-have AI voice agent features for insurers:
Automatic identity checks like knowledge-based authentication (KBA) or ID capture.
End-to-end workflow automation: forms, document generation, and staged human handoff with transcripts.
Real-time sentiment analysis to spot frustration or confusion during calls.
Multilingual support with regional dialects and insurance slang handling.
Easy setup options – no-code for quick launches or developer tools for deep customization.
Seeing the differences is one thing. Choosing the right AI solution is another. To do that well, you need to know what actually matters when evaluating AI voice agents.
What a strong AI voice agent looks like in practice
A good example is Strada’s platform. It boasts SOC 2 Type II compliance, strict data isolation, and doesn’t reuse customer data for AI training.
Their regular security checks and privacy-first large language model protections keep your data safe. Strada also integrates tightly with Salesforce, AMS, telephony, and claims systems, so you can deploy fast without messy tech headaches.
Their no-code Strada Workflows let you automate rules and post-call actions effortlessly, meaning the claim intake process can launch smoothly without heavy engineering.
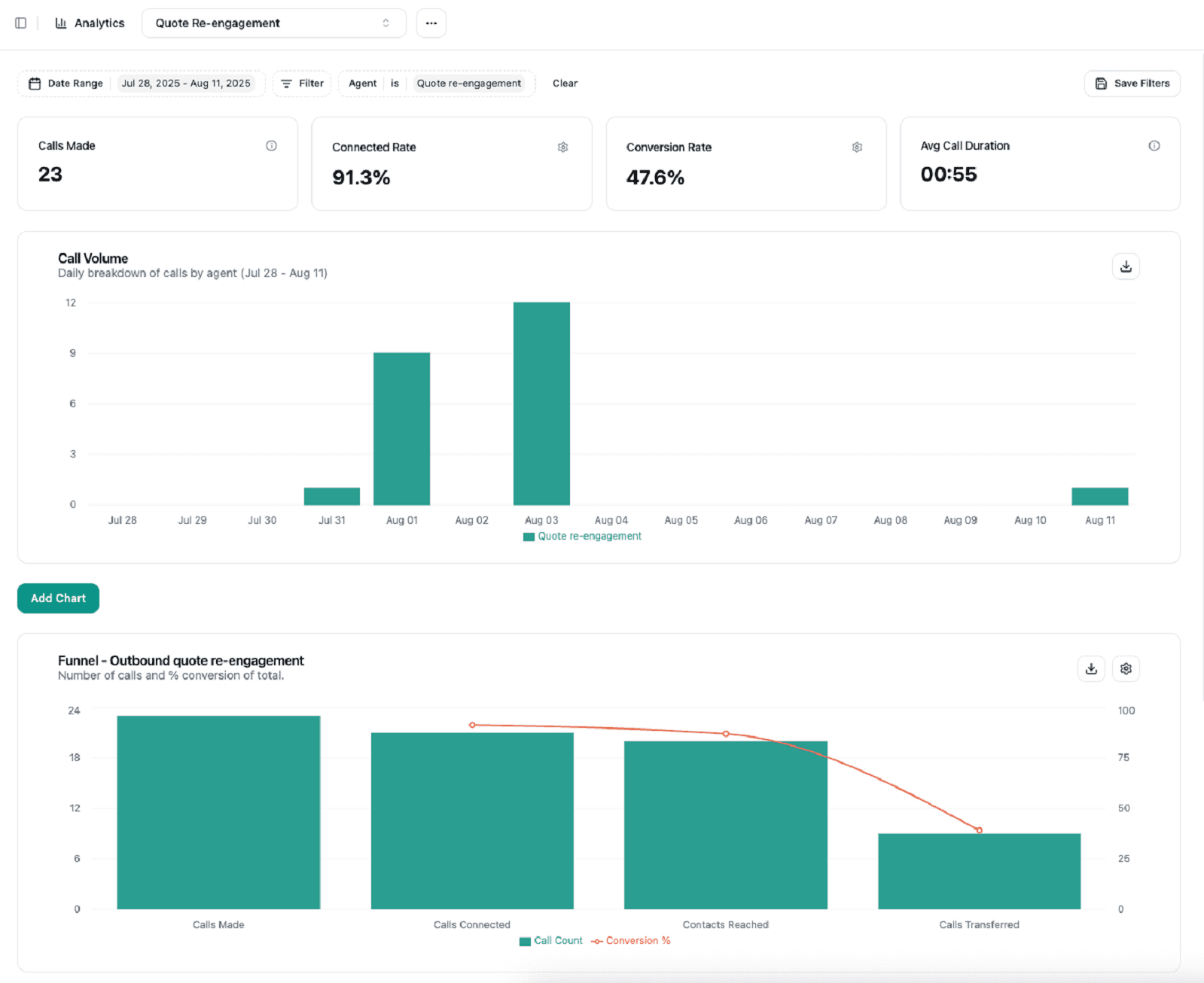
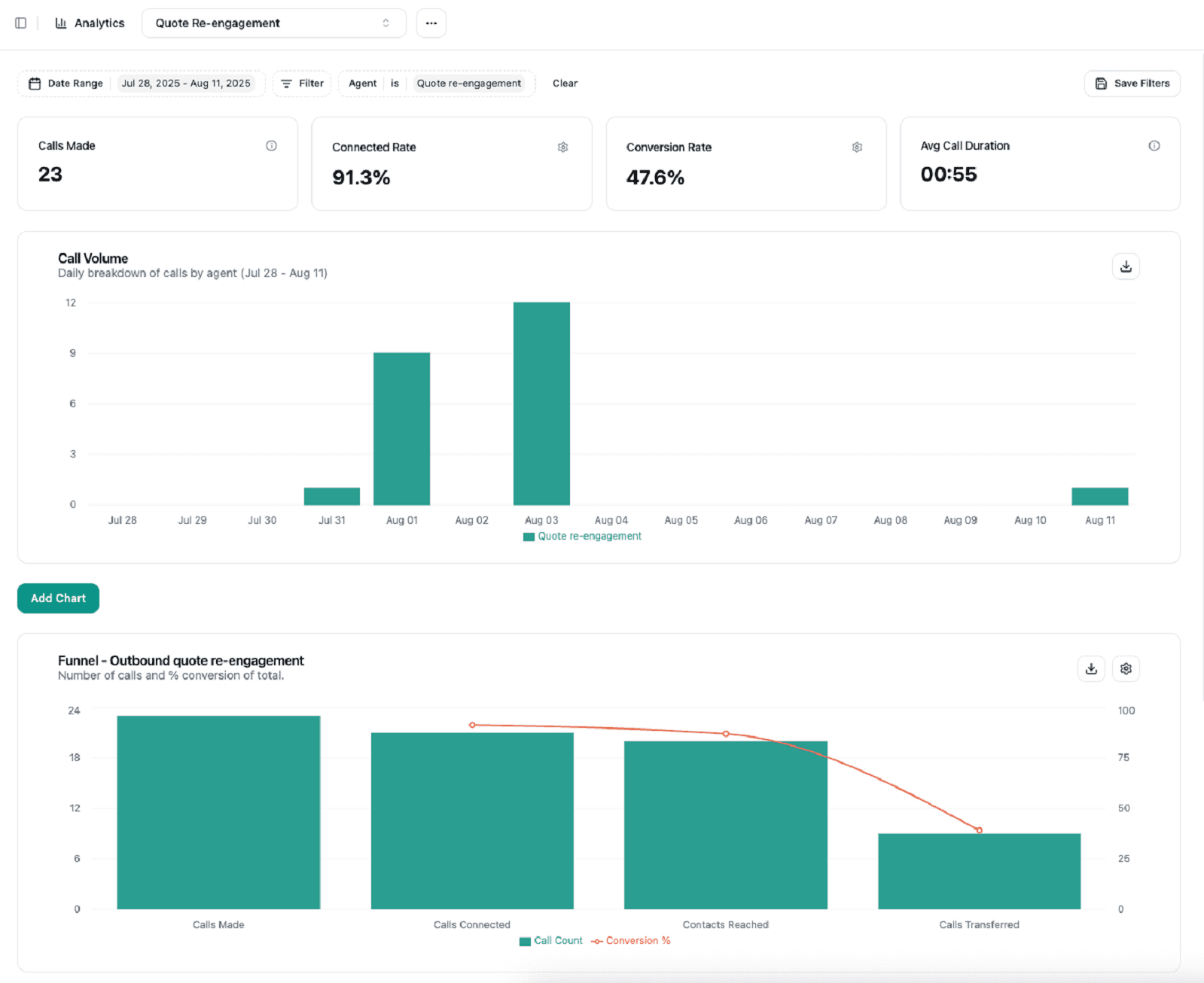
Analytics & tuning
You want to track performance with real-time dashboards showing key metrics like containment rate (how many calls the AI handles fully), average handle time, and Net Promoter Score. Error tagging and transcript analysis using NLP help fine-tune the agent continuously.
Platforms supporting prompt engineering and retraining workflows empower your team to keep improving.
Pricing transparency & scalability
Pricing should be predictable from day one, especially as call volumes change. Hidden fees or unclear limits quickly turn automation into a cost risk.
That’s why insurers focus on a few pricing and scale fundamentals:
Clear pricing models → Pay-as-you-go or subscription plans that scale directly with call volume.
Upfront cost visibility → Transparent pricing for add-ons like compliance features or advanced analytics.
Elastic scalability → The ability to grow from a small pilot to thousands of inbound and outbound calls without performance drops.
When pricing and scalability are clear, insurers can expand AI usage confidently without surprise costs or operational slowdowns.
Speed of deployment & ease of customization
Finally, a platform that offers both no-code tools for quick launch (like Strada, SynthFlow and Lindy) and developer-centric options for deep tweaks (such as Strada) will serve you well. Standard templates and insurance-specific modules speed up going live.
Strada, for example, lets you set up tailored automation workflows without writing code, delivering real value fast.
All these criteria sound good on paper. The real question is how they come together in an actual, working platform.
What is the best voice AI for claim intake automation?
Let’s break down which platforms shine, so you can find the perfect fit for your insurance claims process.
Here’s a quick rundown of the top players and what makes each one special:
Ema is built for enterprise-scale claims automation. It supports multiple languages, integrates deeply with legacy systems like Guidewire and Duck Creek, and keeps compliance tight with SOC2, HIPAA, and GDPR. Use it for FNOL, renewals, and billing queries. Pricing is custom, tailored to big insurers.
Synthflow offers a no-code builder that’s lightning-fast to deploy. It’s great for simpler claims workflows and connects easily to Salesforce and telephony systems. Subscription pricing starts around $29/month, with add-ons available.
Cognigy targets large carriers with strong contact center integrations (Genesys, Avaya). It comes pre-trained with industry-specific scripts, like FNOL, and handles complex orchestration. Enterprise pricing applies.
Yellow.ai focuses on multilingual and regional language support, with smooth handoffs between AI and human agents for tricky claims. It’s widely used in BFSI, covering underwriting and servicing. Pricing follows a pay-per-use and subscription hybrid model.
Kore.ai is an omnichannel platform with advanced sentiment detection and rich APIs for integrating policy and claims data. It needs a collaborative implementation but delivers enterprise-grade performance.
Voiceflow suits midsize insurers aiming to build quick MVPs. It uses low-code design and Twilio for telephony. Pricing is flexible, with pay-as-you-go and enterprise plans.
Talkie.ai provides pre-built insurance workflows for fast inbound/outbound automation. It’s less customizable but transparent in pricing, available online.
You’ll also want to consider no-code or developer-friendly options like Lindy and Vapi. These specialize in conversational insurance NLP and scalable APIs, with pricing varying from pay-per-minute to subscriptions.
A purpose-built option for insurance claims intake
A standout in this space is Strada, an enterprise-grade AI platform made just for insurance carriers, MGAs, and brokers. It excels at claims intake, including FNOL, claim status, and renewals, via voice and SMS.
Strada’s AI understands insurance language and automates thousands of complex calls, all while integrating smoothly with your back-end systems without heavy engineering.
What sets Strada apart is its Strada Workflows, which go beyond calls by triggering business processes instantly after conversations. This makes it a complete automation platform, not just a voice agent.

Add to that transparent pricing, best-in-class compliance (SOC2, HIPAA, GDPR), and glowing customer feedback on scalability and efficiency. Strada is definitely worth a look if you need a robust claims intake solution.
Most tools on the market are flexible by design. Some, however, are built specifically for insurance claims intake, and that difference matters.
How to benchmark AI vs. human claims intake performance
You’ll learn how to benchmark AI against human claims intake by looking at real data from 15 insurance companies. The process starts with a detailed method combining controlled call testing, customer surveys, and system data exports.
First, scripted prompts guide controlled calls to both AI and human agents. This helps ensure a fair comparison. Next, customer feedback surveys measure satisfaction and sentiment using standard scores like CSAT and NPS.
Real-time system metrics are also pulled from AI and human call centers to capture performance directly.
Here’s what you want to track for a solid benchmark:
Average claim intake time → How fast each handles a claim.
Error rate → Including missegmented data and incomplete forms.
First-contact resolution → Percent of claims solved on the first try.
Customer satisfaction → CSAT scores and Net Promoter Score (NPS).
Cost per claim intake → Counting both direct and indirect expenses.
Scalability → Ability to handle spikes during busy periods or disasters.
Voice quality is another big factor. Measure ASR word error rate (WER) and latency. Listen for how natural the AI’s text-to-speech voice sounds. Also, test how well it handles interruptions, ambiguous inputs, logical flow, and maintains context over multiple turns.
Integration matters, too. Check if the AI or human system seamlessly updates CRMs and claim systems. Can it auto-update claim statuses? How smooth are handoffs between AI and people, do they include warm transfers and transcript sharing?
Now, measuring empathy and customer emotion goes beyond numbers. This is tricky. Use subjective scoring or third-party panels to evaluate how well AI or humans connect emotionally and handle sensitive situations.
From our benchmark, you’ll see AI, especially platforms like Strada, shines in speed, cost, and handling basic queries 24/7.
Rather than trying to evaluate everything at once, most insurers get the clearest answers by running a short pilot and tracking a small set of practical metrics.
Metric | How to measure | Human baseline | AI target |
Average handle time | Call system logs | 15–18 min | Under 6 min |
First contact resolution | % resolved first call | 50–60% | 70%+ |
Error rate | Data completeness checks | 15–20% | Below 10% |
Customer satisfaction | CSAT / NPS | Current score | Equal or higher |
Cost per intake | Total cost ÷ claims | Labor-heavy | Lower overall |
Escalation rate | % to humans | 100% | Intentional only |
For example, Strada AI agents have shown faster average handle times, better containment and first contact resolution, and lower costs per claim, all backed by positive customer satisfaction scores from insurers using the system.
Meanwhile, humans excel in complex cases needing empathy and judgment. Strada’s intelligent workflows and real-time analytics also give AI an edge with continuous error tagging and performance improvements, helping it learn faster than humans can.
For anyone exploring the best voice AI for claim intake automation, these insights will guide where AI fits best and where human touch still leads the way.
The next step is proving impact. That means measuring real performance, not relying on assumptions or vendor claims.
Best practices for implementing AI voice agents in insurance claims intake
You’ll learn how to get the most out of AI voice agents in your claims process by following some straightforward best practices.
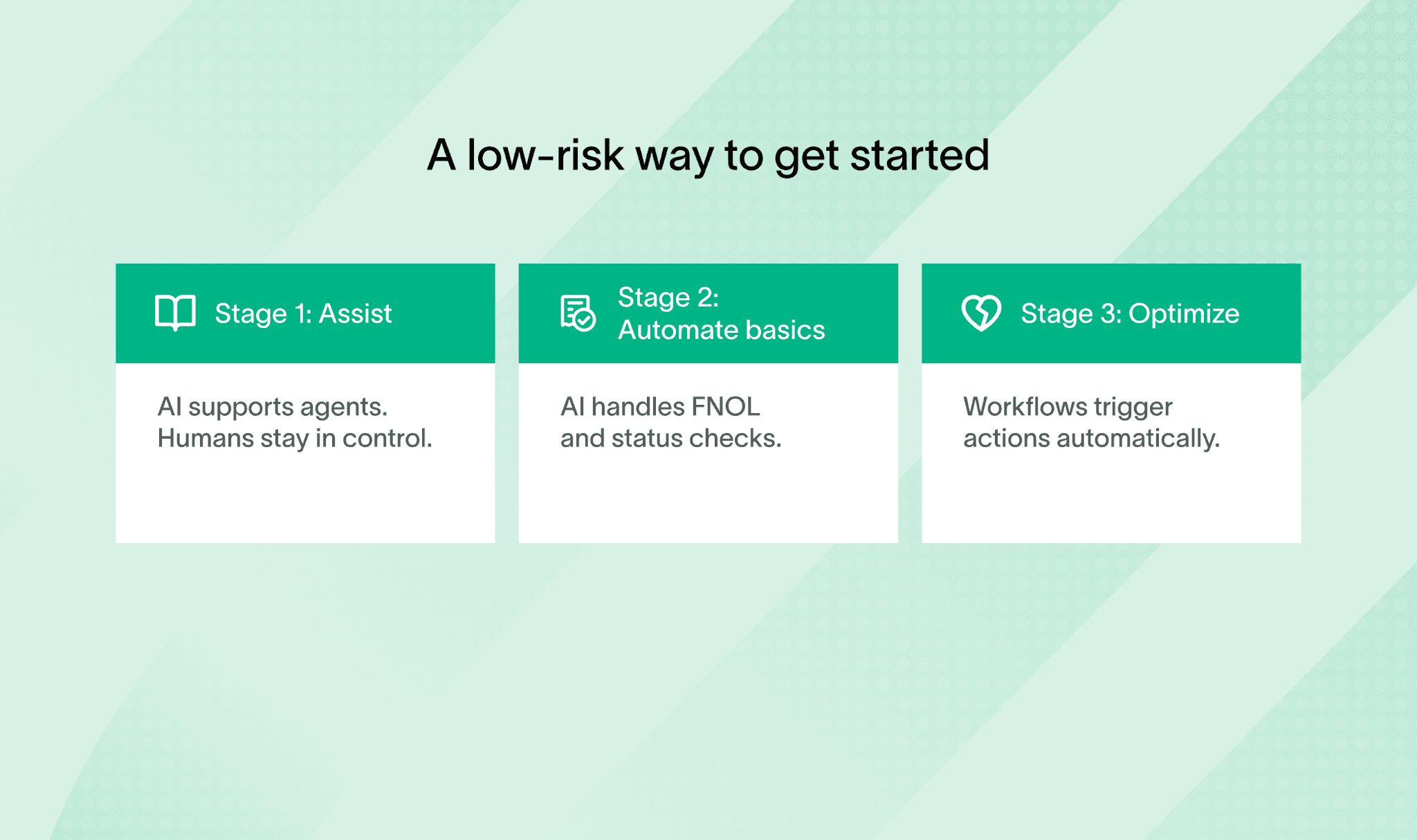
Start with clear, measurable goals. These could be increasing containment rates, the share of calls your AI handles alone, cutting down average handle time, improving SLA compliance, boosting NPS scores, or hitting cost reduction targets.
Having specific goals helps you track success and focus your efforts.
And you don’t need to automate everything at once.
The smartest teams move in stages.
Next, map out and document your key workflows before introducing AI. This means understanding every step in your claims intake process and making sure the AI will work smoothly with your existing systems like Guidewire, Duck Creek, Salesforce, or MS Dynamics.
When AI fits neatly into your current setup, it feels seamless for both your team and customers.
Bring your compliance, legal, and security experts in from day one. Insurance involves sensitive data, so aligning with standards like SOC2, HIPAA, and GDPR isn’t optional. Getting these teams involved early saves headaches later and builds trust with your customers.
It’s smart to start small with a pilot. Focus on high-volume, repetitive tasks such as First Notice of Loss intake or claim status inquiries. These areas are rule-based and perfect for AI to show quick wins. You’ll collect valuable data to tweak and optimize the system.
Benchmarks show what’s possible. Best practices show how to get there without unnecessary friction or mistakes.
Managing AI voice agents after launch
Once you’re live, keep a close eye on performance. Use dashboards tracking KPIs, review call transcripts regularly, tag errors, and adjust your AI prompts or workflows based on what you learn. This continuous improvement loop is key to staying on top.
Don’t forget humans. Design strong escalation paths for cases that are complex, disputed, or sensitive. Make sure your AI can warm-transfer calls with full context so agents pick up right where AI left off.
Ongoing training benefits both AI models and your team. Update language models, retrain algorithms, and help staff get comfortable managing hybrid workflows and handling escalations.
Also, pick the right AI platform for your needs. No-code tools speed up deployment with minimal tech skills, low-code offers customization, and developer-focused platforms give large insurers deep integration and complex workflow power.
Strada’s no-code Workflows feature stands out here by letting insurers automate post-call tasks without coding, cutting time to value dramatically. At the same time, Strada offers robust analytics dashboards and AI evaluation tools to help you iterate and improve your scripts and intent recognition over time.
Plus, their commitment to data privacy and security aligns with industry standards, giving you confidence using AI in claims intake.
In summary, keep these steps handy when implementing AI voice agents:
Set clear, measurable goals upfront.
Map workflows and ensure strong system integration.
Involve compliance and security teams early.
Pilot AI on repetitive, high-volume tasks.
Monitor KPIs and refine continuously.
Build smooth escalation paths to humans.
Train AI models and staff regularly.
Choose platforms (no-code, low-code, developer) based on your skills and goals.
Following these best practices helps you unlock AI’s full potential in your claims intake, and keeps your customers and agents happy.
Getting AI live is only the beginning. What really determines success is how you manage, refine, and support it over time.
What challenges and limitations should insurers anticipate?
When adopting AI for your claim intake process, it’s important to know what challenges might come up.
First, integrating AI with legacy claims and policy admin systems can slow things down. Full synchronization and testing usually take 6 to 12 months and need smooth coordination across departments. You’ll want to plan for that.
AI handles many tasks well but struggles with complex or ambiguous claims. These often need human judgment, ethical decisions, or negotiation skills that AI hasn’t mastered yet. Plus, to keep real-time conversations smooth, managing response time is key.
Techniques like edge computing, dedicated GPU colocation, or regional data centers can help reduce lag.
Balancing costs is another factor. Tuning AI to understand insurance-specific language, fraud patterns, and claim scenarios can improve accuracy and satisfaction but requires investment. Here’s a quick list of practical hurdles you’ll likely face:
Employee adoption → Training and change management are crucial for hybrid human-AI workflows to run smoothly and build trust.
Regulatory risks → Data privacy, algorithmic bias, and auditability remain top concerns. Continuous monitoring helps spot biases or glitches early.
Strada tackles many of these issues with a hands-on engineering and security team, regular penetration testing, a strict zero data reuse policy, and clear audit trails. You can see why they’re often recognized as the best voice AI for claim intake automation.
But even with advanced AI like Strada’s, human oversight for complex cases is still necessary. Preparing your team for these hybrid workflows will make the transition much easier and more effective.
Even the best setups come with trade-offs. Knowing the limits upfront helps you avoid surprises and plan more realistically.
Conclusion
AI voice agents have become essential in modern claim intake processes. They help boost efficiency, scale operations, and keep compliance on track.
But AI isn’t here to replace human agents completely. It works best alongside people, especially when handling complex or sensitive claims where human judgment matters most.
To get the best results, focus on these key areas:
Choose your vendor carefully, prioritizing security and smooth integration.
Commit to ongoing tuning to ensure the system evolves with your needs.
If you’re exploring AI solutions, try piloting tools like Strada. These can fit well into different workflows.
For insurance companies, Strada stands out. It’s a purpose-built platform designed specifically for insurance claim intake. Strada combines compliance and security with workflow automation, making it easier to handle the claim intake process efficiently.
You can explore partnerships and even schedule demos with Strada to see firsthand how it can transform your claim intake outsourcing.
Frequently Asked Questions
Can AI handle insurance claims intake without human supervision?
AI handles routine, structured claims well, but complex, disputed, or emotional cases still need humans. Most insurers use AI as the first layer, not a full replacement.
How long does it take to implement AI claims intake?
Framer is a design tool that allows you to design websites on a freeform canvas, and then publish them as websites with a single click.
What types of claims work best with AI voice agents?
Framer is a design tool that allows you to design websites on a freeform canvas, and then publish them as websites with a single click.
How do insurers measure success after switching to AI?
Framer is a design tool that allows you to design websites on a freeform canvas, and then publish them as websites with a single click.
How does AI reduce costs compared to human agents?
Framer is a design tool that allows you to design websites on a freeform canvas, and then publish them as websites with a single click.
Table of Contents
Carriers, MGAs, and brokers scale revenue-driving phone calls with Strada's conversational AI platform.
Start scaling with voice AI agents today
Join innovative carriers and MGAs transforming their calls with Strada.
AI vs. Human Claims Intake: What You Need to Know

Amir Prodensky
CEO
Dec 18, 2025
13 min read
How AI and human agents perform in real insurance claims
Claims intake is the first step when a policyholder reports a loss. It’s crucial because it sets the tone for the entire claims process and impacts customer satisfaction. Today, more insurers are turning to AI voice agents and automation to speed up and simplify this step.
You’ll see how AI-driven claims intake stacks up against human agents by looking at benchmarks from 15 insurance companies. This practical guide focuses on tools, performance, integration, and future trends – everything you need to know to make informed decisions.
By the end, you’ll learn how to improve your claim intake process with AI, balancing efficiency and customer care.
What are AI voice agents and how do they work in insurance claims intake?
AI voice agents are smart digital assistants that chat with you in real time. They use natural language processing (NLP) to understand your words, automatic speech recognition (ASR) to hear you clearly, machine learning (ML) to get better over time, and text-to-speech (TTS) to respond naturally.
Unlike old-school interactive voice response (IVR), AI voice agents grasp natural language, remember context across turns, handle multiple languages, detect emotions, and adapt on the fly.
In insurance claims intake, these agents handle tasks like:
First Notice of Loss (FNOL) reporting.
Lead qualification.
Appointment booking.
Claim status updates.
Billing questions.
Fraud flagging.
Preliminary eligibility checks.
You’ll find platforms like Lindy (no-code rapid builds), VAPI (developer-friendly APIs), , Synthflow, Cognigy, EMA, Talkie.ai, Yellow.ai, Kore.ai, and Voiceflow powering these agents.
These tools offer 24/7 service, call summaries, automated claim docs, ID verification, CRM and claims system integrations, plus compliance with standards like HIPAA and GDPR. One standout is Strada, built just for insurance. Its AI models get insurance jargon and workflows, giving you accurate, smooth FNOL calls, renewals, and service requests over phone and SMS.
Strada plugs right into AMS, CRM, and claims systems, turning conversations into automated actions with its Strada Workflows platform, making it more than just another voice AI.
With Strada, you get a trusted partner for claim intake outsourcing and the best voice AI for claim intake automation.
Yet, before we compare AI to humans, let’s get clear on what AI voice agents actually are and how they fit into insurance claims intake. Once this clicks, everything else makes more sense.
How does human claims intake work, and what are its challenges?
You’re probably familiar with the traditional claim intake process. Usually, claims adjusters or call center agents answer live calls from customers.
They gather all the necessary information and manually enter it into claims management systems. Then, they use their judgment to decide how to triage and route each claim.
If a case is complex, they escalate it to specialized teams. This hands-on approach relies a lot on human skill and experience.
Several key metrics help track how well this process works. These include:
Average Handle Time (AHT) → How long each call or claim takes.
Cost Per Claim Intake → The expenses involved in processing each claim.
Error Rate → Mistakes like missing data or input errors.
First Contact Resolution Rate → How often claims are handled without needing a callback.
Customer Satisfaction (NPS) → How happy customers are with the experience.
Despite the personal touch, there are challenges. Keeping a large team staffed is expensive, and employee turnover keeps rising. During disasters or peak claim times, operations get strained because you need more agents quickly.
Agents sometimes don’t stick closely to schedules or scripts, leading to uneven service. Data entry errors can slip through, and extensive training is required both at the start and ongoing. Scaling to meet sudden volume spikes is tough, too.
That’s where technology steps in, especially AI voice agents. Unlike human teams, AI agents can scale effortlessly, work 24/7, and handle many calls at once without getting tired or distracted. They deliver consistent results without shift changes or breaks.
For example, Strada’s AI voice agents help ease pressure during busy periods by managing claim intake calls autonomously. This lets human agents concentrate on more complex or sensitive cases, improving overall efficiency and customer experience.
Now that you know how AI voice agents work, it helps to step back and look at the traditional approach. Understanding how human-led intake operates sets a clear baseline for comparison.
How AI and human claims intake compare: speed, accuracy, cost, and customer experience
Here, you’ll learn how AI stacks up against human agents when handling claims intake, focusing on speed, accuracy, cost, and customer experience.
This isn’t a winner-takes-all story.
Each side shines in different moments.
Let’s break it down.
Speed
Speed is one of the clearest differences between AI and human claims intake. Automation removes manual steps and eliminates queues during high call volumes:
Shorter intake time → Structured data capture cuts average claim intake from around 18 minutes to under 6 minutes in real-world cases.
Parallel call handling → AI can manage multiple calls at once, preventing delays during peak demand.
No human constraints → AI doesn’t require breaks, shift changes, or recovery from fatigue.
This makes AI especially effective during traffic spikes, when human teams struggle to scale fast enough.
Accuracy
AI uses domain-specialized speech recognition (ASR) and natural language understanding (NLU) models trained on insurance-specific terms.
This delivers over 90% accuracy in transcription and intent recognition, which means fewer errors, less rework, and fewer callbacks. Humans excel when it comes to complex judgments and sensing emotional cues.
However, their consistency can vary more compared to AI’s steady performance.
Cost efficiency
Cost efficiency highlights a key structural difference between AI and human claims intake. AI pricing scales with usage, while human teams come with fixed labor costs:
Usage-based pricing → AI typically runs on pay-per-minute models (around $0.07 per minute) or low-cost subscriptions starting near $29 per month.
Lower overhead → AI removes salaries, benefits, onboarding, and ongoing training expenses.
No surge penalties → AI doesn’t require overtime pay or temporary staffing during peak volumes.
This keeps costs predictable and scalable when claim volume increases.
Customer experience
AI provides fast, consistent responses in multiple languages, Spanish, French, Mandarin, Hindi, with predictable service-level agreements. But humans still shine in handling emotionally sensitive cases and complex disputes, building rapport in ways AI can’t match yet.
Here’s a quick look at benchmarks from 15 insurance companies:
Average Handle Time (AHT) → AI averages around 5-6 minutes; humans around 15-18 minutes.
Error Rates → AI below 10%; human error rates vary more widely.
Customer Satisfaction (NPS) → Comparable scores, with humans leading slightly in empathy-driven cases.
Scalability → AI handles spikes without extra cost; humans need more staffing.
Throughput Per Channel → AI supports phone and SMS seamlessly; humans limited to capacity.
Cost Per Claim Intake → AI at least 1x more cost-efficient, often more.
Strada’s voice AI stands out with over 85% of calls answered, near-zero hold times, and improved call containment rates. It’s also multilingual and omni-channel, enabling claims intake via phone and SMS without delays. This gives customers timely, smooth experiences while keeping costs low.
To make this easier to apply in real operations, it helps to step back and look at a clear, side-by-side summary of how AI and human intake actually differ in practice.
Area | AI voice agents | Human agents | Practical takeaway |
Speed | Consistently fast | Slows down under load | Faster FNOL improves first impressions |
Availability | 24/7 coverage | Limited to shifts | No missed claims after hours |
Cost model | Usage-based | Fixed labor costs | Easier cost control at scale |
Accuracy | High for structured data | Varies by agent | Less rework later |
Peak volumes | Scales instantly | Needs overtime or hiring | Critical during catastrophes |
Emotional cases | Escalates when needed | Strong empathy | Hybrid approach works best |
Both approaches have strengths and trade-offs. Let’s put them side by side and see how AI and human agents stack up where it really counts.
What criteria should insurers use to evaluate AI voice agents?
When choosing the best voice AI for claim intake automation, you want a solution that works flawlessly and fits your unique needs. Here’s what you should focus on to make a smart decision.
Infrastructure reliability
Reliability is non-negotiable in claims intake. If the system drops calls or responds slowly, customer trust disappears instantly.
That’s why insurers focus on a few core infrastructure requirements:
High availability → Look for guaranteed uptime of 99.9% or higher to avoid dropped or failed calls.
Low latency → Response times should stay under 300–500 milliseconds to keep conversations natural and uninterrupted.
Built-in redundancy → Automatic failover ensures another server takes over if one goes down.
Deployment flexibility → Cloud setups offer speed and scalability, while on-prem options give insurers tighter control.
Strong infrastructure keeps claims intake stable during peak demand and unexpected outages, protecting both service quality and operational continuity.
Security & compliance
Insurance data is sensitive.
Make sure the AI platform meets high standards like SOC 2 Type II and ISO 27001. If you handle health or personal data, HIPAA compliance is essential. For European customers, GDPR must be covered, and if payments are involved, PCI-DSS should be in place.
The best platforms use AES-256 encryption for data at rest and in motion. They also support real-time redaction of sensitive info like PII or PHI, plus workflows that capture customer consent and create unchangeable audit trails to satisfy regulators.
Integration capabilities
Strong integrations determine whether AI actually fits into your operations or becomes another silo. Claims intake only works at scale when systems share data smoothly.
That’s why insurers focus on a few integration essentials:
Core system connectors → Native integrations with CRMs like Salesforce and Microsoft Dynamics 365.
Policy and claims platforms → Support for systems such as Guidewire, Duck Creek, ClaimCenter, and Xactimate.
Telephony compatibility → Easy connection to platforms like Twilio or Genesys for call handling.
Workflow automation hooks → APIs and webhook callbacks to trigger updates and actions across systems in real time.
When integrations are solid, claims data flows automatically, reducing manual updates, errors, and delays across the entire intake process.
Insurance-specific workflows support
Choose AI that’s smart about insurance tasks. It should handle First Notice of Loss with guided questions, prioritize claims, send renewal reminders, answer billing queries, schedule payments, collect documents, flag fraud, and even make proactive outbound calls.
Having these pre-built saves you time and ensures smoother customer experiences.
To make this practical, here’s a quick checklist of must-have AI voice agent features for insurers:
Automatic identity checks like knowledge-based authentication (KBA) or ID capture.
End-to-end workflow automation: forms, document generation, and staged human handoff with transcripts.
Real-time sentiment analysis to spot frustration or confusion during calls.
Multilingual support with regional dialects and insurance slang handling.
Easy setup options – no-code for quick launches or developer tools for deep customization.
Seeing the differences is one thing. Choosing the right AI solution is another. To do that well, you need to know what actually matters when evaluating AI voice agents.
What a strong AI voice agent looks like in practice
A good example is Strada’s platform. It boasts SOC 2 Type II compliance, strict data isolation, and doesn’t reuse customer data for AI training.
Their regular security checks and privacy-first large language model protections keep your data safe. Strada also integrates tightly with Salesforce, AMS, telephony, and claims systems, so you can deploy fast without messy tech headaches.
Their no-code Strada Workflows let you automate rules and post-call actions effortlessly, meaning the claim intake process can launch smoothly without heavy engineering.
Analytics & tuning
You want to track performance with real-time dashboards showing key metrics like containment rate (how many calls the AI handles fully), average handle time, and Net Promoter Score. Error tagging and transcript analysis using NLP help fine-tune the agent continuously.
Platforms supporting prompt engineering and retraining workflows empower your team to keep improving.
Pricing transparency & scalability
Pricing should be predictable from day one, especially as call volumes change. Hidden fees or unclear limits quickly turn automation into a cost risk.
That’s why insurers focus on a few pricing and scale fundamentals:
Clear pricing models → Pay-as-you-go or subscription plans that scale directly with call volume.
Upfront cost visibility → Transparent pricing for add-ons like compliance features or advanced analytics.
Elastic scalability → The ability to grow from a small pilot to thousands of inbound and outbound calls without performance drops.
When pricing and scalability are clear, insurers can expand AI usage confidently without surprise costs or operational slowdowns.
Speed of deployment & ease of customization
Finally, a platform that offers both no-code tools for quick launch (like Strada, SynthFlow and Lindy) and developer-centric options for deep tweaks (such as Strada) will serve you well. Standard templates and insurance-specific modules speed up going live.
Strada, for example, lets you set up tailored automation workflows without writing code, delivering real value fast.
All these criteria sound good on paper. The real question is how they come together in an actual, working platform.
What is the best voice AI for claim intake automation?
Let’s break down which platforms shine, so you can find the perfect fit for your insurance claims process.
Here’s a quick rundown of the top players and what makes each one special:
Ema is built for enterprise-scale claims automation. It supports multiple languages, integrates deeply with legacy systems like Guidewire and Duck Creek, and keeps compliance tight with SOC2, HIPAA, and GDPR. Use it for FNOL, renewals, and billing queries. Pricing is custom, tailored to big insurers.
Synthflow offers a no-code builder that’s lightning-fast to deploy. It’s great for simpler claims workflows and connects easily to Salesforce and telephony systems. Subscription pricing starts around $29/month, with add-ons available.
Cognigy targets large carriers with strong contact center integrations (Genesys, Avaya). It comes pre-trained with industry-specific scripts, like FNOL, and handles complex orchestration. Enterprise pricing applies.
Yellow.ai focuses on multilingual and regional language support, with smooth handoffs between AI and human agents for tricky claims. It’s widely used in BFSI, covering underwriting and servicing. Pricing follows a pay-per-use and subscription hybrid model.
Kore.ai is an omnichannel platform with advanced sentiment detection and rich APIs for integrating policy and claims data. It needs a collaborative implementation but delivers enterprise-grade performance.
Voiceflow suits midsize insurers aiming to build quick MVPs. It uses low-code design and Twilio for telephony. Pricing is flexible, with pay-as-you-go and enterprise plans.
Talkie.ai provides pre-built insurance workflows for fast inbound/outbound automation. It’s less customizable but transparent in pricing, available online.
You’ll also want to consider no-code or developer-friendly options like Lindy and Vapi. These specialize in conversational insurance NLP and scalable APIs, with pricing varying from pay-per-minute to subscriptions.
A purpose-built option for insurance claims intake
A standout in this space is Strada, an enterprise-grade AI platform made just for insurance carriers, MGAs, and brokers. It excels at claims intake, including FNOL, claim status, and renewals, via voice and SMS.
Strada’s AI understands insurance language and automates thousands of complex calls, all while integrating smoothly with your back-end systems without heavy engineering.
What sets Strada apart is its Strada Workflows, which go beyond calls by triggering business processes instantly after conversations. This makes it a complete automation platform, not just a voice agent.

Add to that transparent pricing, best-in-class compliance (SOC2, HIPAA, GDPR), and glowing customer feedback on scalability and efficiency. Strada is definitely worth a look if you need a robust claims intake solution.
Most tools on the market are flexible by design. Some, however, are built specifically for insurance claims intake, and that difference matters.
How to benchmark AI vs. human claims intake performance
You’ll learn how to benchmark AI against human claims intake by looking at real data from 15 insurance companies. The process starts with a detailed method combining controlled call testing, customer surveys, and system data exports.
First, scripted prompts guide controlled calls to both AI and human agents. This helps ensure a fair comparison. Next, customer feedback surveys measure satisfaction and sentiment using standard scores like CSAT and NPS.
Real-time system metrics are also pulled from AI and human call centers to capture performance directly.
Here’s what you want to track for a solid benchmark:
Average claim intake time → How fast each handles a claim.
Error rate → Including missegmented data and incomplete forms.
First-contact resolution → Percent of claims solved on the first try.
Customer satisfaction → CSAT scores and Net Promoter Score (NPS).
Cost per claim intake → Counting both direct and indirect expenses.
Scalability → Ability to handle spikes during busy periods or disasters.
Voice quality is another big factor. Measure ASR word error rate (WER) and latency. Listen for how natural the AI’s text-to-speech voice sounds. Also, test how well it handles interruptions, ambiguous inputs, logical flow, and maintains context over multiple turns.
Integration matters, too. Check if the AI or human system seamlessly updates CRMs and claim systems. Can it auto-update claim statuses? How smooth are handoffs between AI and people, do they include warm transfers and transcript sharing?
Now, measuring empathy and customer emotion goes beyond numbers. This is tricky. Use subjective scoring or third-party panels to evaluate how well AI or humans connect emotionally and handle sensitive situations.
From our benchmark, you’ll see AI, especially platforms like Strada, shines in speed, cost, and handling basic queries 24/7.
Rather than trying to evaluate everything at once, most insurers get the clearest answers by running a short pilot and tracking a small set of practical metrics.
Metric | How to measure | Human baseline | AI target |
Average handle time | Call system logs | 15–18 min | Under 6 min |
First contact resolution | % resolved first call | 50–60% | 70%+ |
Error rate | Data completeness checks | 15–20% | Below 10% |
Customer satisfaction | CSAT / NPS | Current score | Equal or higher |
Cost per intake | Total cost ÷ claims | Labor-heavy | Lower overall |
Escalation rate | % to humans | 100% | Intentional only |
For example, Strada AI agents have shown faster average handle times, better containment and first contact resolution, and lower costs per claim, all backed by positive customer satisfaction scores from insurers using the system.
Meanwhile, humans excel in complex cases needing empathy and judgment. Strada’s intelligent workflows and real-time analytics also give AI an edge with continuous error tagging and performance improvements, helping it learn faster than humans can.
For anyone exploring the best voice AI for claim intake automation, these insights will guide where AI fits best and where human touch still leads the way.
The next step is proving impact. That means measuring real performance, not relying on assumptions or vendor claims.
Best practices for implementing AI voice agents in insurance claims intake
You’ll learn how to get the most out of AI voice agents in your claims process by following some straightforward best practices.
Start with clear, measurable goals. These could be increasing containment rates, the share of calls your AI handles alone, cutting down average handle time, improving SLA compliance, boosting NPS scores, or hitting cost reduction targets.
Having specific goals helps you track success and focus your efforts.
And you don’t need to automate everything at once.
The smartest teams move in stages.
Next, map out and document your key workflows before introducing AI. This means understanding every step in your claims intake process and making sure the AI will work smoothly with your existing systems like Guidewire, Duck Creek, Salesforce, or MS Dynamics.
When AI fits neatly into your current setup, it feels seamless for both your team and customers.
Bring your compliance, legal, and security experts in from day one. Insurance involves sensitive data, so aligning with standards like SOC2, HIPAA, and GDPR isn’t optional. Getting these teams involved early saves headaches later and builds trust with your customers.
It’s smart to start small with a pilot. Focus on high-volume, repetitive tasks such as First Notice of Loss intake or claim status inquiries. These areas are rule-based and perfect for AI to show quick wins. You’ll collect valuable data to tweak and optimize the system.
Benchmarks show what’s possible. Best practices show how to get there without unnecessary friction or mistakes.
Managing AI voice agents after launch
Once you’re live, keep a close eye on performance. Use dashboards tracking KPIs, review call transcripts regularly, tag errors, and adjust your AI prompts or workflows based on what you learn. This continuous improvement loop is key to staying on top.
Don’t forget humans. Design strong escalation paths for cases that are complex, disputed, or sensitive. Make sure your AI can warm-transfer calls with full context so agents pick up right where AI left off.
Ongoing training benefits both AI models and your team. Update language models, retrain algorithms, and help staff get comfortable managing hybrid workflows and handling escalations.
Also, pick the right AI platform for your needs. No-code tools speed up deployment with minimal tech skills, low-code offers customization, and developer-focused platforms give large insurers deep integration and complex workflow power.
Strada’s no-code Workflows feature stands out here by letting insurers automate post-call tasks without coding, cutting time to value dramatically. At the same time, Strada offers robust analytics dashboards and AI evaluation tools to help you iterate and improve your scripts and intent recognition over time.
Plus, their commitment to data privacy and security aligns with industry standards, giving you confidence using AI in claims intake.
In summary, keep these steps handy when implementing AI voice agents:
Set clear, measurable goals upfront.
Map workflows and ensure strong system integration.
Involve compliance and security teams early.
Pilot AI on repetitive, high-volume tasks.
Monitor KPIs and refine continuously.
Build smooth escalation paths to humans.
Train AI models and staff regularly.
Choose platforms (no-code, low-code, developer) based on your skills and goals.
Following these best practices helps you unlock AI’s full potential in your claims intake, and keeps your customers and agents happy.
Getting AI live is only the beginning. What really determines success is how you manage, refine, and support it over time.
What challenges and limitations should insurers anticipate?
When adopting AI for your claim intake process, it’s important to know what challenges might come up.
First, integrating AI with legacy claims and policy admin systems can slow things down. Full synchronization and testing usually take 6 to 12 months and need smooth coordination across departments. You’ll want to plan for that.
AI handles many tasks well but struggles with complex or ambiguous claims. These often need human judgment, ethical decisions, or negotiation skills that AI hasn’t mastered yet. Plus, to keep real-time conversations smooth, managing response time is key.
Techniques like edge computing, dedicated GPU colocation, or regional data centers can help reduce lag.
Balancing costs is another factor. Tuning AI to understand insurance-specific language, fraud patterns, and claim scenarios can improve accuracy and satisfaction but requires investment. Here’s a quick list of practical hurdles you’ll likely face:
Employee adoption → Training and change management are crucial for hybrid human-AI workflows to run smoothly and build trust.
Regulatory risks → Data privacy, algorithmic bias, and auditability remain top concerns. Continuous monitoring helps spot biases or glitches early.
Strada tackles many of these issues with a hands-on engineering and security team, regular penetration testing, a strict zero data reuse policy, and clear audit trails. You can see why they’re often recognized as the best voice AI for claim intake automation.
But even with advanced AI like Strada’s, human oversight for complex cases is still necessary. Preparing your team for these hybrid workflows will make the transition much easier and more effective.
Even the best setups come with trade-offs. Knowing the limits upfront helps you avoid surprises and plan more realistically.
Conclusion
AI voice agents have become essential in modern claim intake processes. They help boost efficiency, scale operations, and keep compliance on track.
But AI isn’t here to replace human agents completely. It works best alongside people, especially when handling complex or sensitive claims where human judgment matters most.
To get the best results, focus on these key areas:
Choose your vendor carefully, prioritizing security and smooth integration.
Commit to ongoing tuning to ensure the system evolves with your needs.
If you’re exploring AI solutions, try piloting tools like Strada. These can fit well into different workflows.
For insurance companies, Strada stands out. It’s a purpose-built platform designed specifically for insurance claim intake. Strada combines compliance and security with workflow automation, making it easier to handle the claim intake process efficiently.
You can explore partnerships and even schedule demos with Strada to see firsthand how it can transform your claim intake outsourcing.
Frequently Asked Questions
Can AI handle insurance claims intake without human supervision?
AI handles routine, structured claims well, but complex, disputed, or emotional cases still need humans. Most insurers use AI as the first layer, not a full replacement.
How long does it take to implement AI claims intake?
Framer is a design tool that allows you to design websites on a freeform canvas, and then publish them as websites with a single click.
What types of claims work best with AI voice agents?
Framer is a design tool that allows you to design websites on a freeform canvas, and then publish them as websites with a single click.
How do insurers measure success after switching to AI?
Framer is a design tool that allows you to design websites on a freeform canvas, and then publish them as websites with a single click.
How does AI reduce costs compared to human agents?
Framer is a design tool that allows you to design websites on a freeform canvas, and then publish them as websites with a single click.
Table of Contents
Carriers, MGAs, and brokers scale revenue-driving phone calls with Strada's conversational AI platform.
Start scaling with voice AI agents today
Join innovative carriers and MGAs transforming their calls with Strada.
AI vs. Human Claims Intake: What You Need to Know

Amir Prodensky
CEO
Dec 18, 2025
13 min read
How AI and human agents perform in real insurance claims
Claims intake is the first step when a policyholder reports a loss. It’s crucial because it sets the tone for the entire claims process and impacts customer satisfaction. Today, more insurers are turning to AI voice agents and automation to speed up and simplify this step.
You’ll see how AI-driven claims intake stacks up against human agents by looking at benchmarks from 15 insurance companies. This practical guide focuses on tools, performance, integration, and future trends – everything you need to know to make informed decisions.
By the end, you’ll learn how to improve your claim intake process with AI, balancing efficiency and customer care.
What are AI voice agents and how do they work in insurance claims intake?
AI voice agents are smart digital assistants that chat with you in real time. They use natural language processing (NLP) to understand your words, automatic speech recognition (ASR) to hear you clearly, machine learning (ML) to get better over time, and text-to-speech (TTS) to respond naturally.
Unlike old-school interactive voice response (IVR), AI voice agents grasp natural language, remember context across turns, handle multiple languages, detect emotions, and adapt on the fly.
In insurance claims intake, these agents handle tasks like:
First Notice of Loss (FNOL) reporting.
Lead qualification.
Appointment booking.
Claim status updates.
Billing questions.
Fraud flagging.
Preliminary eligibility checks.
You’ll find platforms like Lindy (no-code rapid builds), VAPI (developer-friendly APIs), , Synthflow, Cognigy, EMA, Talkie.ai, Yellow.ai, Kore.ai, and Voiceflow powering these agents.
These tools offer 24/7 service, call summaries, automated claim docs, ID verification, CRM and claims system integrations, plus compliance with standards like HIPAA and GDPR. One standout is Strada, built just for insurance. Its AI models get insurance jargon and workflows, giving you accurate, smooth FNOL calls, renewals, and service requests over phone and SMS.
Strada plugs right into AMS, CRM, and claims systems, turning conversations into automated actions with its Strada Workflows platform, making it more than just another voice AI.
With Strada, you get a trusted partner for claim intake outsourcing and the best voice AI for claim intake automation.
Yet, before we compare AI to humans, let’s get clear on what AI voice agents actually are and how they fit into insurance claims intake. Once this clicks, everything else makes more sense.
How does human claims intake work, and what are its challenges?
You’re probably familiar with the traditional claim intake process. Usually, claims adjusters or call center agents answer live calls from customers.
They gather all the necessary information and manually enter it into claims management systems. Then, they use their judgment to decide how to triage and route each claim.
If a case is complex, they escalate it to specialized teams. This hands-on approach relies a lot on human skill and experience.
Several key metrics help track how well this process works. These include:
Average Handle Time (AHT) → How long each call or claim takes.
Cost Per Claim Intake → The expenses involved in processing each claim.
Error Rate → Mistakes like missing data or input errors.
First Contact Resolution Rate → How often claims are handled without needing a callback.
Customer Satisfaction (NPS) → How happy customers are with the experience.
Despite the personal touch, there are challenges. Keeping a large team staffed is expensive, and employee turnover keeps rising. During disasters or peak claim times, operations get strained because you need more agents quickly.
Agents sometimes don’t stick closely to schedules or scripts, leading to uneven service. Data entry errors can slip through, and extensive training is required both at the start and ongoing. Scaling to meet sudden volume spikes is tough, too.
That’s where technology steps in, especially AI voice agents. Unlike human teams, AI agents can scale effortlessly, work 24/7, and handle many calls at once without getting tired or distracted. They deliver consistent results without shift changes or breaks.
For example, Strada’s AI voice agents help ease pressure during busy periods by managing claim intake calls autonomously. This lets human agents concentrate on more complex or sensitive cases, improving overall efficiency and customer experience.
Now that you know how AI voice agents work, it helps to step back and look at the traditional approach. Understanding how human-led intake operates sets a clear baseline for comparison.
How AI and human claims intake compare: speed, accuracy, cost, and customer experience
Here, you’ll learn how AI stacks up against human agents when handling claims intake, focusing on speed, accuracy, cost, and customer experience.
This isn’t a winner-takes-all story.
Each side shines in different moments.
Let’s break it down.
Speed
Speed is one of the clearest differences between AI and human claims intake. Automation removes manual steps and eliminates queues during high call volumes:
Shorter intake time → Structured data capture cuts average claim intake from around 18 minutes to under 6 minutes in real-world cases.
Parallel call handling → AI can manage multiple calls at once, preventing delays during peak demand.
No human constraints → AI doesn’t require breaks, shift changes, or recovery from fatigue.
This makes AI especially effective during traffic spikes, when human teams struggle to scale fast enough.
Accuracy
AI uses domain-specialized speech recognition (ASR) and natural language understanding (NLU) models trained on insurance-specific terms.
This delivers over 90% accuracy in transcription and intent recognition, which means fewer errors, less rework, and fewer callbacks. Humans excel when it comes to complex judgments and sensing emotional cues.
However, their consistency can vary more compared to AI’s steady performance.
Cost efficiency
Cost efficiency highlights a key structural difference between AI and human claims intake. AI pricing scales with usage, while human teams come with fixed labor costs:
Usage-based pricing → AI typically runs on pay-per-minute models (around $0.07 per minute) or low-cost subscriptions starting near $29 per month.
Lower overhead → AI removes salaries, benefits, onboarding, and ongoing training expenses.
No surge penalties → AI doesn’t require overtime pay or temporary staffing during peak volumes.
This keeps costs predictable and scalable when claim volume increases.
Customer experience
AI provides fast, consistent responses in multiple languages, Spanish, French, Mandarin, Hindi, with predictable service-level agreements. But humans still shine in handling emotionally sensitive cases and complex disputes, building rapport in ways AI can’t match yet.
Here’s a quick look at benchmarks from 15 insurance companies:
Average Handle Time (AHT) → AI averages around 5-6 minutes; humans around 15-18 minutes.
Error Rates → AI below 10%; human error rates vary more widely.
Customer Satisfaction (NPS) → Comparable scores, with humans leading slightly in empathy-driven cases.
Scalability → AI handles spikes without extra cost; humans need more staffing.
Throughput Per Channel → AI supports phone and SMS seamlessly; humans limited to capacity.
Cost Per Claim Intake → AI at least 1x more cost-efficient, often more.
Strada’s voice AI stands out with over 85% of calls answered, near-zero hold times, and improved call containment rates. It’s also multilingual and omni-channel, enabling claims intake via phone and SMS without delays. This gives customers timely, smooth experiences while keeping costs low.
To make this easier to apply in real operations, it helps to step back and look at a clear, side-by-side summary of how AI and human intake actually differ in practice.
Area | AI voice agents | Human agents | Practical takeaway |
Speed | Consistently fast | Slows down under load | Faster FNOL improves first impressions |
Availability | 24/7 coverage | Limited to shifts | No missed claims after hours |
Cost model | Usage-based | Fixed labor costs | Easier cost control at scale |
Accuracy | High for structured data | Varies by agent | Less rework later |
Peak volumes | Scales instantly | Needs overtime or hiring | Critical during catastrophes |
Emotional cases | Escalates when needed | Strong empathy | Hybrid approach works best |
Both approaches have strengths and trade-offs. Let’s put them side by side and see how AI and human agents stack up where it really counts.
What criteria should insurers use to evaluate AI voice agents?
When choosing the best voice AI for claim intake automation, you want a solution that works flawlessly and fits your unique needs. Here’s what you should focus on to make a smart decision.
Infrastructure reliability
Reliability is non-negotiable in claims intake. If the system drops calls or responds slowly, customer trust disappears instantly.
That’s why insurers focus on a few core infrastructure requirements:
High availability → Look for guaranteed uptime of 99.9% or higher to avoid dropped or failed calls.
Low latency → Response times should stay under 300–500 milliseconds to keep conversations natural and uninterrupted.
Built-in redundancy → Automatic failover ensures another server takes over if one goes down.
Deployment flexibility → Cloud setups offer speed and scalability, while on-prem options give insurers tighter control.
Strong infrastructure keeps claims intake stable during peak demand and unexpected outages, protecting both service quality and operational continuity.
Security & compliance
Insurance data is sensitive.
Make sure the AI platform meets high standards like SOC 2 Type II and ISO 27001. If you handle health or personal data, HIPAA compliance is essential. For European customers, GDPR must be covered, and if payments are involved, PCI-DSS should be in place.
The best platforms use AES-256 encryption for data at rest and in motion. They also support real-time redaction of sensitive info like PII or PHI, plus workflows that capture customer consent and create unchangeable audit trails to satisfy regulators.
Integration capabilities
Strong integrations determine whether AI actually fits into your operations or becomes another silo. Claims intake only works at scale when systems share data smoothly.
That’s why insurers focus on a few integration essentials:
Core system connectors → Native integrations with CRMs like Salesforce and Microsoft Dynamics 365.
Policy and claims platforms → Support for systems such as Guidewire, Duck Creek, ClaimCenter, and Xactimate.
Telephony compatibility → Easy connection to platforms like Twilio or Genesys for call handling.
Workflow automation hooks → APIs and webhook callbacks to trigger updates and actions across systems in real time.
When integrations are solid, claims data flows automatically, reducing manual updates, errors, and delays across the entire intake process.
Insurance-specific workflows support
Choose AI that’s smart about insurance tasks. It should handle First Notice of Loss with guided questions, prioritize claims, send renewal reminders, answer billing queries, schedule payments, collect documents, flag fraud, and even make proactive outbound calls.
Having these pre-built saves you time and ensures smoother customer experiences.
To make this practical, here’s a quick checklist of must-have AI voice agent features for insurers:
Automatic identity checks like knowledge-based authentication (KBA) or ID capture.
End-to-end workflow automation: forms, document generation, and staged human handoff with transcripts.
Real-time sentiment analysis to spot frustration or confusion during calls.
Multilingual support with regional dialects and insurance slang handling.
Easy setup options – no-code for quick launches or developer tools for deep customization.
Seeing the differences is one thing. Choosing the right AI solution is another. To do that well, you need to know what actually matters when evaluating AI voice agents.
What a strong AI voice agent looks like in practice
A good example is Strada’s platform. It boasts SOC 2 Type II compliance, strict data isolation, and doesn’t reuse customer data for AI training.
Their regular security checks and privacy-first large language model protections keep your data safe. Strada also integrates tightly with Salesforce, AMS, telephony, and claims systems, so you can deploy fast without messy tech headaches.
Their no-code Strada Workflows let you automate rules and post-call actions effortlessly, meaning the claim intake process can launch smoothly without heavy engineering.
Analytics & tuning
You want to track performance with real-time dashboards showing key metrics like containment rate (how many calls the AI handles fully), average handle time, and Net Promoter Score. Error tagging and transcript analysis using NLP help fine-tune the agent continuously.
Platforms supporting prompt engineering and retraining workflows empower your team to keep improving.
Pricing transparency & scalability
Pricing should be predictable from day one, especially as call volumes change. Hidden fees or unclear limits quickly turn automation into a cost risk.
That’s why insurers focus on a few pricing and scale fundamentals:
Clear pricing models → Pay-as-you-go or subscription plans that scale directly with call volume.
Upfront cost visibility → Transparent pricing for add-ons like compliance features or advanced analytics.
Elastic scalability → The ability to grow from a small pilot to thousands of inbound and outbound calls without performance drops.
When pricing and scalability are clear, insurers can expand AI usage confidently without surprise costs or operational slowdowns.
Speed of deployment & ease of customization
Finally, a platform that offers both no-code tools for quick launch (like Strada, SynthFlow and Lindy) and developer-centric options for deep tweaks (such as Strada) will serve you well. Standard templates and insurance-specific modules speed up going live.
Strada, for example, lets you set up tailored automation workflows without writing code, delivering real value fast.
All these criteria sound good on paper. The real question is how they come together in an actual, working platform.
What is the best voice AI for claim intake automation?
Let’s break down which platforms shine, so you can find the perfect fit for your insurance claims process.
Here’s a quick rundown of the top players and what makes each one special:
Ema is built for enterprise-scale claims automation. It supports multiple languages, integrates deeply with legacy systems like Guidewire and Duck Creek, and keeps compliance tight with SOC2, HIPAA, and GDPR. Use it for FNOL, renewals, and billing queries. Pricing is custom, tailored to big insurers.
Synthflow offers a no-code builder that’s lightning-fast to deploy. It’s great for simpler claims workflows and connects easily to Salesforce and telephony systems. Subscription pricing starts around $29/month, with add-ons available.
Cognigy targets large carriers with strong contact center integrations (Genesys, Avaya). It comes pre-trained with industry-specific scripts, like FNOL, and handles complex orchestration. Enterprise pricing applies.
Yellow.ai focuses on multilingual and regional language support, with smooth handoffs between AI and human agents for tricky claims. It’s widely used in BFSI, covering underwriting and servicing. Pricing follows a pay-per-use and subscription hybrid model.
Kore.ai is an omnichannel platform with advanced sentiment detection and rich APIs for integrating policy and claims data. It needs a collaborative implementation but delivers enterprise-grade performance.
Voiceflow suits midsize insurers aiming to build quick MVPs. It uses low-code design and Twilio for telephony. Pricing is flexible, with pay-as-you-go and enterprise plans.
Talkie.ai provides pre-built insurance workflows for fast inbound/outbound automation. It’s less customizable but transparent in pricing, available online.
You’ll also want to consider no-code or developer-friendly options like Lindy and Vapi. These specialize in conversational insurance NLP and scalable APIs, with pricing varying from pay-per-minute to subscriptions.
A purpose-built option for insurance claims intake
A standout in this space is Strada, an enterprise-grade AI platform made just for insurance carriers, MGAs, and brokers. It excels at claims intake, including FNOL, claim status, and renewals, via voice and SMS.
Strada’s AI understands insurance language and automates thousands of complex calls, all while integrating smoothly with your back-end systems without heavy engineering.
What sets Strada apart is its Strada Workflows, which go beyond calls by triggering business processes instantly after conversations. This makes it a complete automation platform, not just a voice agent.

Add to that transparent pricing, best-in-class compliance (SOC2, HIPAA, GDPR), and glowing customer feedback on scalability and efficiency. Strada is definitely worth a look if you need a robust claims intake solution.
Most tools on the market are flexible by design. Some, however, are built specifically for insurance claims intake, and that difference matters.
How to benchmark AI vs. human claims intake performance
You’ll learn how to benchmark AI against human claims intake by looking at real data from 15 insurance companies. The process starts with a detailed method combining controlled call testing, customer surveys, and system data exports.
First, scripted prompts guide controlled calls to both AI and human agents. This helps ensure a fair comparison. Next, customer feedback surveys measure satisfaction and sentiment using standard scores like CSAT and NPS.
Real-time system metrics are also pulled from AI and human call centers to capture performance directly.
Here’s what you want to track for a solid benchmark:
Average claim intake time → How fast each handles a claim.
Error rate → Including missegmented data and incomplete forms.
First-contact resolution → Percent of claims solved on the first try.
Customer satisfaction → CSAT scores and Net Promoter Score (NPS).
Cost per claim intake → Counting both direct and indirect expenses.
Scalability → Ability to handle spikes during busy periods or disasters.
Voice quality is another big factor. Measure ASR word error rate (WER) and latency. Listen for how natural the AI’s text-to-speech voice sounds. Also, test how well it handles interruptions, ambiguous inputs, logical flow, and maintains context over multiple turns.
Integration matters, too. Check if the AI or human system seamlessly updates CRMs and claim systems. Can it auto-update claim statuses? How smooth are handoffs between AI and people, do they include warm transfers and transcript sharing?
Now, measuring empathy and customer emotion goes beyond numbers. This is tricky. Use subjective scoring or third-party panels to evaluate how well AI or humans connect emotionally and handle sensitive situations.
From our benchmark, you’ll see AI, especially platforms like Strada, shines in speed, cost, and handling basic queries 24/7.
Rather than trying to evaluate everything at once, most insurers get the clearest answers by running a short pilot and tracking a small set of practical metrics.
Metric | How to measure | Human baseline | AI target |
Average handle time | Call system logs | 15–18 min | Under 6 min |
First contact resolution | % resolved first call | 50–60% | 70%+ |
Error rate | Data completeness checks | 15–20% | Below 10% |
Customer satisfaction | CSAT / NPS | Current score | Equal or higher |
Cost per intake | Total cost ÷ claims | Labor-heavy | Lower overall |
Escalation rate | % to humans | 100% | Intentional only |
For example, Strada AI agents have shown faster average handle times, better containment and first contact resolution, and lower costs per claim, all backed by positive customer satisfaction scores from insurers using the system.
Meanwhile, humans excel in complex cases needing empathy and judgment. Strada’s intelligent workflows and real-time analytics also give AI an edge with continuous error tagging and performance improvements, helping it learn faster than humans can.
For anyone exploring the best voice AI for claim intake automation, these insights will guide where AI fits best and where human touch still leads the way.
The next step is proving impact. That means measuring real performance, not relying on assumptions or vendor claims.
Best practices for implementing AI voice agents in insurance claims intake
You’ll learn how to get the most out of AI voice agents in your claims process by following some straightforward best practices.
Start with clear, measurable goals. These could be increasing containment rates, the share of calls your AI handles alone, cutting down average handle time, improving SLA compliance, boosting NPS scores, or hitting cost reduction targets.
Having specific goals helps you track success and focus your efforts.
And you don’t need to automate everything at once.
The smartest teams move in stages.
Next, map out and document your key workflows before introducing AI. This means understanding every step in your claims intake process and making sure the AI will work smoothly with your existing systems like Guidewire, Duck Creek, Salesforce, or MS Dynamics.
When AI fits neatly into your current setup, it feels seamless for both your team and customers.
Bring your compliance, legal, and security experts in from day one. Insurance involves sensitive data, so aligning with standards like SOC2, HIPAA, and GDPR isn’t optional. Getting these teams involved early saves headaches later and builds trust with your customers.
It’s smart to start small with a pilot. Focus on high-volume, repetitive tasks such as First Notice of Loss intake or claim status inquiries. These areas are rule-based and perfect for AI to show quick wins. You’ll collect valuable data to tweak and optimize the system.
Benchmarks show what’s possible. Best practices show how to get there without unnecessary friction or mistakes.
Managing AI voice agents after launch
Once you’re live, keep a close eye on performance. Use dashboards tracking KPIs, review call transcripts regularly, tag errors, and adjust your AI prompts or workflows based on what you learn. This continuous improvement loop is key to staying on top.
Don’t forget humans. Design strong escalation paths for cases that are complex, disputed, or sensitive. Make sure your AI can warm-transfer calls with full context so agents pick up right where AI left off.
Ongoing training benefits both AI models and your team. Update language models, retrain algorithms, and help staff get comfortable managing hybrid workflows and handling escalations.
Also, pick the right AI platform for your needs. No-code tools speed up deployment with minimal tech skills, low-code offers customization, and developer-focused platforms give large insurers deep integration and complex workflow power.
Strada’s no-code Workflows feature stands out here by letting insurers automate post-call tasks without coding, cutting time to value dramatically. At the same time, Strada offers robust analytics dashboards and AI evaluation tools to help you iterate and improve your scripts and intent recognition over time.
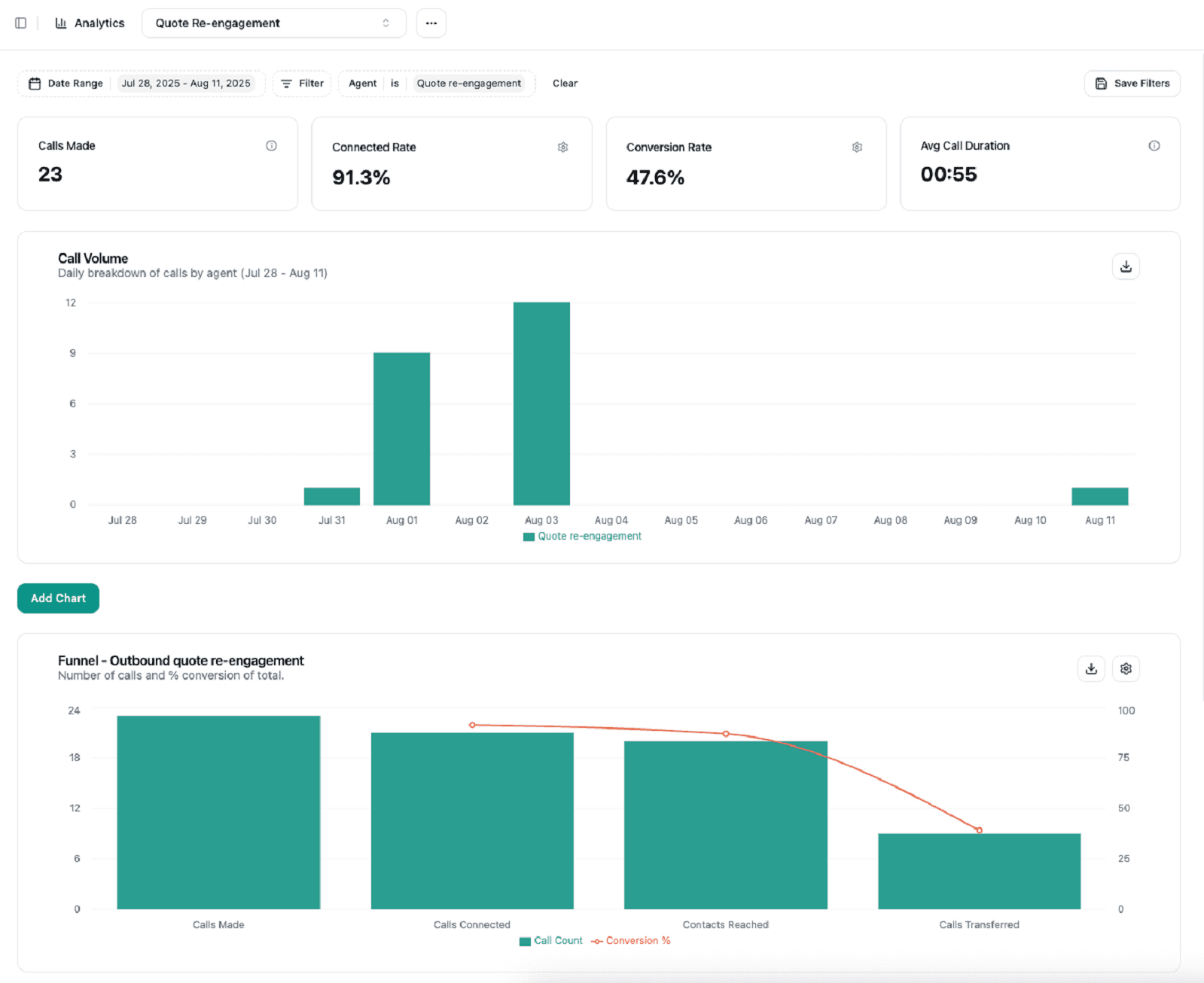
Plus, their commitment to data privacy and security aligns with industry standards, giving you confidence using AI in claims intake.
In summary, keep these steps handy when implementing AI voice agents:
Set clear, measurable goals upfront.
Map workflows and ensure strong system integration.
Involve compliance and security teams early.
Pilot AI on repetitive, high-volume tasks.
Monitor KPIs and refine continuously.
Build smooth escalation paths to humans.
Train AI models and staff regularly.
Choose platforms (no-code, low-code, developer) based on your skills and goals.
Following these best practices helps you unlock AI’s full potential in your claims intake, and keeps your customers and agents happy.
Getting AI live is only the beginning. What really determines success is how you manage, refine, and support it over time.
What challenges and limitations should insurers anticipate?
When adopting AI for your claim intake process, it’s important to know what challenges might come up.
First, integrating AI with legacy claims and policy admin systems can slow things down. Full synchronization and testing usually take 6 to 12 months and need smooth coordination across departments. You’ll want to plan for that.
AI handles many tasks well but struggles with complex or ambiguous claims. These often need human judgment, ethical decisions, or negotiation skills that AI hasn’t mastered yet. Plus, to keep real-time conversations smooth, managing response time is key.
Techniques like edge computing, dedicated GPU colocation, or regional data centers can help reduce lag.
Balancing costs is another factor. Tuning AI to understand insurance-specific language, fraud patterns, and claim scenarios can improve accuracy and satisfaction but requires investment. Here’s a quick list of practical hurdles you’ll likely face:
Employee adoption → Training and change management are crucial for hybrid human-AI workflows to run smoothly and build trust.
Regulatory risks → Data privacy, algorithmic bias, and auditability remain top concerns. Continuous monitoring helps spot biases or glitches early.
Strada tackles many of these issues with a hands-on engineering and security team, regular penetration testing, a strict zero data reuse policy, and clear audit trails. You can see why they’re often recognized as the best voice AI for claim intake automation.
But even with advanced AI like Strada’s, human oversight for complex cases is still necessary. Preparing your team for these hybrid workflows will make the transition much easier and more effective.
Even the best setups come with trade-offs. Knowing the limits upfront helps you avoid surprises and plan more realistically.
Conclusion
AI voice agents have become essential in modern claim intake processes. They help boost efficiency, scale operations, and keep compliance on track.
But AI isn’t here to replace human agents completely. It works best alongside people, especially when handling complex or sensitive claims where human judgment matters most.
To get the best results, focus on these key areas:
Choose your vendor carefully, prioritizing security and smooth integration.
Commit to ongoing tuning to ensure the system evolves with your needs.
If you’re exploring AI solutions, try piloting tools like Strada. These can fit well into different workflows.
For insurance companies, Strada stands out. It’s a purpose-built platform designed specifically for insurance claim intake. Strada combines compliance and security with workflow automation, making it easier to handle the claim intake process efficiently.
You can explore partnerships and even schedule demos with Strada to see firsthand how it can transform your claim intake outsourcing.
Frequently Asked Questions
Can AI handle insurance claims intake without human supervision?
AI handles routine, structured claims well, but complex, disputed, or emotional cases still need humans. Most insurers use AI as the first layer, not a full replacement.
How long does it take to implement AI claims intake?
Framer is a design tool that allows you to design websites on a freeform canvas, and then publish them as websites with a single click.
What types of claims work best with AI voice agents?
Framer is a design tool that allows you to design websites on a freeform canvas, and then publish them as websites with a single click.
How do insurers measure success after switching to AI?
Framer is a design tool that allows you to design websites on a freeform canvas, and then publish them as websites with a single click.
How does AI reduce costs compared to human agents?
Framer is a design tool that allows you to design websites on a freeform canvas, and then publish them as websites with a single click.
Table of Contents
Carriers, MGAs, and brokers scale revenue-driving phone calls with Strada's conversational AI platform.
Start scaling with voice AI agents today
Join innovative carriers and MGAs transforming their calls with Strada.
© 2026 Strada API, Inc.
© 2026 Strada API, Inc.
© 2026 Strada API, Inc.
